There are several reasons for a tooth to be extracted (extensive decay, advanced periodontal disease, fractures that advance subgingivally, etc). Extracting a tooth is a relatively simple and fast healing procedure. After surgery and before healing, a blood clot is formed inside the cavity that acts to protect the bone and the nerve endings.
However, there may be problems with healing, causing a complication called alveolitis. This word is the result of the union of two terms: alveolus and “ite”. Alveolus is the cavity that supports the root of the teeth and “ite” means inflammation/infection.
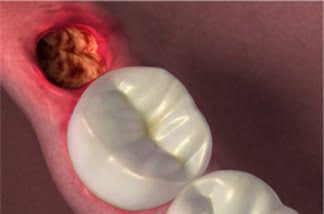
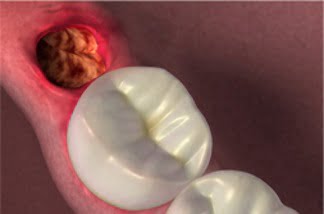
In alveolitis, either the blood clot dislodges, being broken up, or it is not formed properly, exposing the bone to possible infectious agents.
Usually alveolitis occurs 2 to 5 days after the extraction surgery, and the patient reports pain and bad breath. The most recurrent cases of the disease occur in third molar alveoli.
Pre-existing infections, contraceptives, vigorous swishing during the first few hours after extraction, poor irrigation during surgery, lack of wound care, and smoking increase the chances of occurrence. It is also more prevalent in women.
Types of Alveolitis
There are two types of alveolitis: dry and wet. The dryness is due to the clot not forming or dissolving, keeping the cavity empty and without any kind of protection, resulting in pain and discomfort. The wet one has coagulum formation along with a purulent collection within the alveolus. Due to the pus, the clot is dark in color, the patient reports severe pain and a bad odor.
It can be prevented if there is some care, such as:
- Perform liquid and paste diet in the first 24 hours after the procedure;
- Do not rinse frequently and vigorously;
- If you are a smoker, stop smoking for at least 24 hours.
- Do not eat hard foods in the first few days after surgery;
- Use mouthwash with proven antibacterial effect, but do not rinse vigorously;
- If possible stay at rest.
For treatment, it is necessary for the patient to see a dentist. Antinflammatories and antibiotics are prescribed in order to combat infection and relieve pain. Through treatment, the necrotic bone is dissolved and replaced by a healthy one, this period of elimination of the disease usually occurs within three weeks.
If it is a dry alveolitis, an anesthetic can be used to momentarily relieve the pain. In both types of alveolitis, the suture must be removed so that the cavity can be cleaned with chlorhexidine and saline.
In addition to the use of antibiotics and analgesics, the necrotic tissue must be removed with curettes and a re-evaluation done after 48 hours. There is also intra-alveolar medication, which acts as a buffer and contributes to regeneration. These medicines are made from eugenol and propolis.
After the intervention in the infected alveolus, you should not eat and drink hot food or touch the wound with any instruments.
Intra-Alveolar Medication
Alveolar dressings such as Alveosan and Alveolex are commonly used as local analgesics and are not known for their restorative action.
To treat alveolitis, it is necessary to fight the infection and use dressings that help the repair process.
A research was done with the objective of verifying the effectiveness of alveolar dressings not only their antiseptic function, but also as an accelerator agent of the reparative process of alveolitis.
Using two groups of rats, which had teeth extracted and alveolitis caused in the laboratory, the reparative properties of the drug “Alveosan” were evaluated.
In the first group, therapeutic treatment with the alveolar dressing was not performed. Result: necrotic tissue remained for up to nine days, resorption began on day 6, and bone tissue only began to be neoformed on day 15.
In the second group (that was applied the drug “Alveosan”), there was no necrotic tissue recorded from day 3, where there was already resorption, and from day 5, neoformed bone tissues were recorded.
Another research study, which looked at the types of alveolitis treatments used by a group of dental surgeons, found that when there is only the application of intra-alveolar medication, there is acceleration in alveolar repair compared to no treatment. However, when associated with surgical cleaning, even better results are obtained. The dressing with the greatest biocompatibility and effectiveness is “Alveosan”.
Questions asked on the Internet about alveolitis
1 – Hello! I had my molar (26) extracted, and after the extraction I suffered from dry alveolitis, a lot of pain, and a large cavity was left where a bovine bone graft would be performed with a subsequent dental implant. Can an implant be performed? Does it take time to heal? Is a removable prosthesis worth it?
Re: Good afternoon,
What’s up?
Graft and implant only after the alveolitis is resolved. The dentist must make an evaluation of the site, once the site is covered with gum and there are no signs of infection, he must evaluate the need or not for grafting through a tomography taken 3 months after the extraction. There are 3 possible situations:
– If there is enough bone to surround the entire implant with a safety margin, you don’t need a graft.
– If there is enough bone for good implant locking but not enough for complete implant involvement, the graft can be performed in the same session as the implant.
– If there is not enough bone to get even the locking of the implant, the graft must be done first, the healing must wait, and after this period, it is reevaluated, and if there is enough bone, the implant is installed.
The removable prosthesis can be used as long as it does not touch the gum in the region of the graft and/or implant.
Att, Dr. Josué.
Scientific paper summary on Alveolitis
INTRODUCTION
Dry socket or alveolar osteitis is the most common post-extraction complication in dentistry. Dry socket is an extraction socket with exposed bone, devoid of a blood clot, and it may be filled with food debris, edema of the surrounding gingiva, and regional lymphadenitis. There are many predisposing factors for the formation of a dry socket such as complexity and pain during surgery, fragments of root or bone remaining in the wound, vasoconstrictors in local anesthetic solutions, oral contraceptives use, smoking, the surgeons’ expertise, and poor oral hygiene. The management of alveolar osteitis involves controlling the pain until normal healing begins.
MATERIALS AND METHODS
This quasi-experimental trial was conducted in the dental department of Lahore General Hospital from March 2016 till February 2017. Ethical approval was taken from the hospital review committee. The WHO sample size calculator was used for sample size estimation. Considering a 5% level of significance, 80% power, anticipated sample and population proportions of 6% and 27%, a sample size of 96 was estimated to be adequate. All 20-40 years aged patients that reported to the dental department with a painful mandibular molar, were indicated to have an extraction, had a history of good oral hygiene and no systemic disease were invited to participate in the study.
RESULT
There were a total of 96 patients in the study with 48 in each group. The mean age of the patients was 29.53 + 4.95 years. The occurrence of blood clot disintegration was compared between the two groups on day 5. A significantly greater proportion of disintegrated blood clots were found in the control group (n = 17, 35.4%) as compared to the propolis (n = 4, 8.3%) group. The occurrence of exposed bone was compared between the two groups on days 1 and 5. On day 1, a greater number of patients from the propolis group had exposed bone (n = 42, 87.5%), as compared to the control group (n = 34, 70.8%). However, the trend was reversed on the next follow-up. On day 5, a greater number of patients from the control group had exposed bone (n = 17, 35.4%), as compared to the Propolis group (n = 4, 8.3%).
DISCUSSION
Alveolar osteitis is a widely studied post-op complication in dentistry. Numerous studies have been conducted to find the safest and most effective method of preventing and treating the condition. One of the major challenges faced in identifying dry sockets is an inconsistent definition and lack of standardized diagnostic criteria. Since dry socket is one of the most common post-extraction complications, it is imperative to understand the pathology, prevention, and treatment. Literature highlights the need to establish a uniform definition of dry sockets and to critically review the etiology and pathogenesis of the condition. Moreover, there is a dire need to identify and eliminate potential risk factors and improve preventive strategies against alveolar osteitis.
CONCLUSION
In conclusion, this study aimed to evaluate the effectiveness of propolis gel in reducing the occurrence of dry sockets after the extraction of mandibular molar teeth. The results showed that the use of propolis gel significantly reduced the occurrence of disintegrated blood clots and exposed bone, indicating its potential as a preventive measure for dry socket. Further empirical evidence is required to establish the biologically plausible role of propolis gel in the prevention of dry sockets after tooth extractions.
Source: https://journalofkcd.com/index.php/pmsrj/article/view/13